What is Diabetes? Symptoms, Causes, Complications, and Management
Posted by Prescription Hope - See Editorial Guidelines (Last Updated On: Fri Jul 14 2023)
Diabetes is a complex medical condition that can affect many different aspects of your health and life. In this article, we dive into every aspect of diabetes and what you need to know and do to ensure your condition is being well controlled.
Here is a quick summary to get our brains turning, then we will dive into more details.
What is Diabetes? Diabetes is a group of diseases that affect the pancreas and the body’s cell’s response to insulin. It causes high blood sugar, which, if left untreated, can cause other health complications that can be life-threatening. There are different types of diabetes, which each has different causes and treatment methods.
With this brief explanation in mind, let’s cover the specifics surrounding diabetes.
The basics of diabetes
Diabetes is a group of medical conditions directly dealing with the pancreas, insulin, cells, and blood sugar.
Insulin is a hormone produced by the pancreas. It works with the cells of the body as a lock-and-key mechanism.
After consuming carbohydrates, your body will break down the carbs and turn them into glucose. The glucose enters the bloodstream. Insulin will then attach to cells triggering them to uptake the glucose. The glucose can then be used as fuel for the body to function.
With diabetes, though, something goes array. Either not enough insulin is being produced, or the body’s cells are not responding to insulin correctly. Therefore, glucose remains in the bloodstream.
This buildup of glucose, referred to as high blood sugar (hyperglycemia), can then cause damage to nerves, arteries, and organs.
Types of diabetes
Diabetes is considered a group of diseases because there are different types of diabetes. Here is a breakdown of each type and its respective description.
Prediabetes
Roughly one-third of the American population is considered prediabetic. Having prediabetes means that your blood sugar is higher than normal, but it is not high enough to be considered full-blown type 2 diabetes.
Typically, someone with a fasting blood sugar level between 100-125 mg/dL is considered prediabetic. Individuals that have prediabetes can prevent their condition from progressing by making certain lifestyle changes.
Type 2 Diabetes
Type 2 diabetes, which may be referred to as adult-onset diabetes, often follows the prediabetes stage. This is when your fasting blood glucose level exceeds 126 mg/dL.
This form of diabetes is often caused by lifestyle choices that result in your cells becoming resistant to insulin. However, it can also result in the pancreas not producing enough insulin to keep blood glucose levels under control.
In recent years, more and more children have been diagnosed with type 2 diabetes due to the rise of childhood obesity.
Type 1 Diabetes
Type 1 diabetes, often called juvenile diabetes, is an autoimmune condition. This means that the immune system mistakenly attacks itself. In this case, the immune system begins to attack insulin-producing cells, resulting in a loss of insulin production.
Typically, type 1 diabetes is diagnosed during childhood or teenage years. Those that have this type of diabetes require insulin injections to control their blood sugar levels.
Gestational Diabetes
Gestational diabetes refers to one’s blood sugar levels becoming high during pregnancy. Roughly 10% of pregnant women are affected by gestational diabetes in the US each year.
This type occurs because the woman’s pancreas cannot produce enough insulin to keep up with the glucose buildup caused by the hormones in the placenta. Women with gestational diabetes should strive to reach these blood sugar guidelines set forth by the American Diabetes Association (ADA).
- 95 mg/dL or less before a meal
- 140 mg/dL or less an hour after a meal
- 120 mg/dL or less two hours after a meal
Type 1.5 Diabetes
Type 1.5 diabetes is a subtype of type 1 diabetes that is also called latent autoimmune diabetes in adults (LADA). This type has similarities of both type 1 and type 2, as its onset begins like type 2 diabetes.
However, one’s beta cells begin to stop functioning properly much more quickly when compared to type 2 diabetes. Many patients with type 1.5 diabetes are often misdiagnosed with type 2 at first and may be given a treatment recommendation that will soon not fit their needs.
Signs and symptoms of diabetes
The signs and symptoms of diabetes are very similar across the different types, as they are related to high blood sugar. However, the symptoms of type 2 and type 1.5 may be more subtle, and the onset of them may not be as quick as type 1 diabetes.
Here is a list of symptoms to look for:
- Frequent urination
- Fatigue
- Tiredness
- Feeling of extreme thirst
- Blurred vision
- Unexplained weight loss
- Feeling of hunger
- Slow-healing wounds
- Tingling or numbness in hands or feet
- Dry mouth
- Nausea
- Irritability
- Presence of ketones in the urine
What to do if you are newly diagnosed
Receiving a new diagnosis of anything can be overwhelming. Getting diagnosed with diabetes can leave you asking a thousand questions and wondering how to even manage the condition.
Luckily the American Diabetes Association offers resources, such as finding a diabetes educator in your area.
Your doctor will also be able to offer you resources for educating yourself about how to control your condition properly and the effects that diabetes can have on your health.
The best thing you can do after getting diagnosed with diabetes is to continue to follow up with your doctor, learn everything you can, and monitor your blood sugar carefully.
Connection between diabetes and other conditions
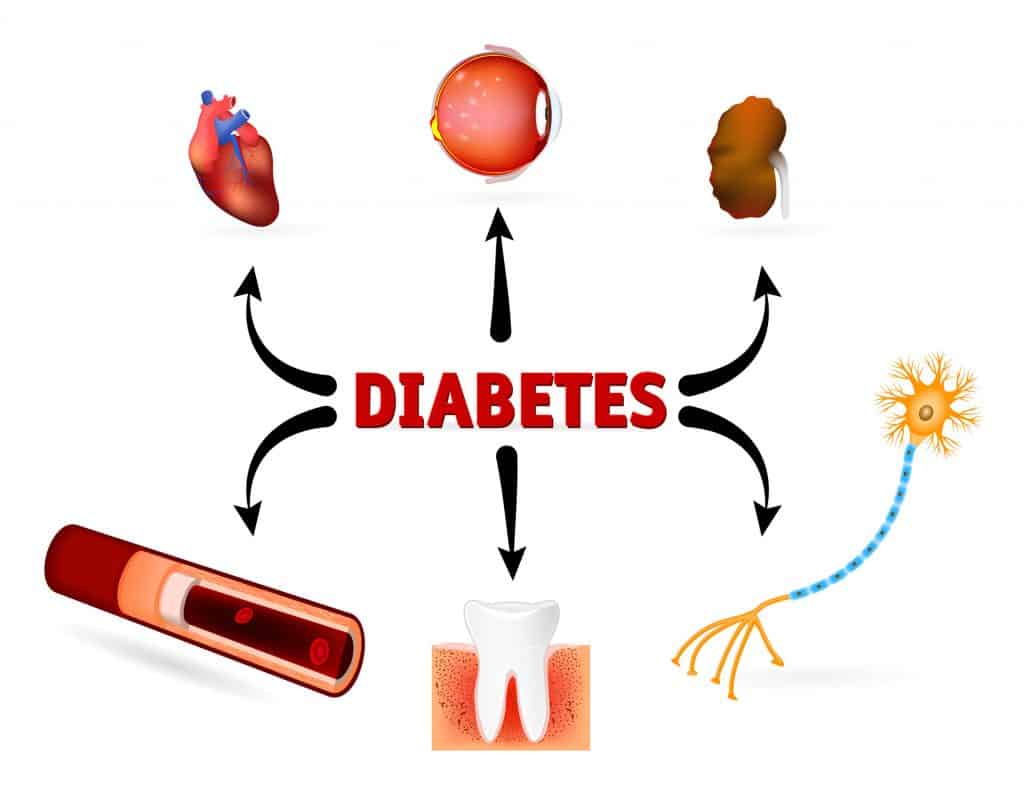
Untreated or poorly managed diabetes can lead to other health complications, which can be life-threatening at times. Here is a list of other conditions that can be exacerbated by uncontrolled blood sugar levels.
Cardiovascular Disease
Cardiovascular disease, or heart disease, is an umbrella term covering a wide variety of problems associated with the heart. When a person with diabetes has long-term uncontrolled blood sugar levels, the arteries and blood vessels can experience plaque buildup.
Plaque buildup can put a person at an increased risk of having a heart attack or stroke. It is no wonder that many patients with diabetes pass away due to a heart-related condition.
Eye Problems
Around 40-45% of Americans with diabetes end up having eye problems, often called diabetic retinopathy.
Chronically high blood sugar can damage the eyes’ small blood vessels, causing fluid to leak into the retina. This then leads to inflammation, causing blurry vision.
Glaucoma and cataracts are two common eye conditions associated with diabetes.
Kidney Problems
The longer that a person has diabetes, the greater their risk is of having kidney problems (nephropathy).
High blood sugar levels can cause the blood vessels in the kidneys to become narrowed and blocked. This can injure kidney tissue and cause increased blood pressure throughout the body.
Nerves in the kidneys and bladder can also be damaged. This may cause a patient to not know their bladder is full because messages are not transmitted correctly to the brain. This can lead to pressure placed on the kidneys and an increased risk of a urinary tract infection (UTI).
Neuropathy
Neuropathy refers to a disease of one or more peripheral nerves, which often causes numbness and weakness. It is estimated that as many as 50% of people with diabetes are affected by neuropathy.
Diabetic neuropathy will often affect the nerves of the legs and feet, causing pain, tingling or burning sensation, and foot problems, such as ulcers and infections.
This type of nerve damage can also affect your digestive system, urinary tract, blood vessels, and heart.
Osteoporosis
Osteoporosis is a condition that is characterized by weakened and less dense bones, putting a person at an increased risk of fractures.
Individuals with diabetes have been shown to have lower bone density and poorer bone health. This may be due to inflammation often associated with hyperglycemia, as well as vitamin D deficiency that is often present in those with diabetes.
Alzheimer’s
It is believed that both diabetes and Alzheimer’s can worsen the condition of the other. The exact link is not fully known, but it may have to do with how hyperglycemia from diabetes damages blood vessels and could potentially reduce blood flow to the brain.
Reduced blood flow to the brain means that the brain is not getting enough nutrients. This can lead to cognitive impairment.
Gum Disease
Uncontrolled blood sugar levels can lead to an increased risk of bacterial infections of the mouth.
Gum disease is just one of the multiple dental health problems that can be associated with diabetes.
Factors that affect blood glucose control
One misconception about diabetes is that only the carbohydrates you eat affect your blood sugar control.
Though the carbs in your food is one main variable that needs to be considered, many other factors can impact one’s blood glucose control. Here is a breakdown of all the different factors.
- Food
- The type of carbohydrates you eat will affect your glucose control differently. There is a difference between complex and simple carbohydrates. Simple carbs are more likely to cause a dramatic, rapid spike in blood sugar levels.
- Proteins and fats can affect blood sugar by minimally increasing levels and helping stabilize sugar throughout the day.
- Alcohol can affect your control by causing either spikes or drops in glucose levels.
- Caffeine intake from coffee or other drinks may also spike blood sugar levels.
- Medication
- The timing and dose of your insulin or other diabetes medication may cause fluctuations in your blood sugar, depending on your treatment method.
- Certain medications taken for other conditions can also negatively affect your glucose control. Patients should consult their doctor for advice to determine which medications can make it harder to control their diabetes condition.
- Exercise
- Different types of exercises will affect your blood sugar differently. However, most exercises will increase insulin sensitivity and aid in glucose control.
- The timing of your food and insulin dosages around your exercise will also have an effect.
- Biological
- Biological hormones can dramatically impact your blood sugar levels. Hormones are often impacted by the amount of sleep you get, stress levels, illnesses, injuries, allergies, and puberty. Hormones can also cause the dawn phenomenon (high blood sugar in the morning).
- Lifestyle Choices
- Lifestyle choices, such as smoking, can lead to worsened insulin resistance and worsened blood sugar control.
Medicines that treat diabetes
Now that you know what diabetes is and the many nuances surrounding it, let’s cover ways to treat the condition.
Many different medicines are used to treat the different types of diabetes. The most popular prescription drug would have to be insulin.
Type 1 diabetes patients must use insulin to control their condition, and those with type 2 may be able to use another medication.

There are a variety of different types of insulin, all of which serve a different purpose. For example, long-acting insulin is often injected just once a day and helps control blood sugar levels between meals and throughout the night.
Short-acting, also referred to as rapid-acting insulin, is often administered to cover meals, snacks, and blood sugar corrections.
Check out our article covering the different types of insulin more in-depth.
There are many oral medications for treating type 2 and some injectable medicines. Again, depending on the severity of your condition, some type 2 diabetes patients may need insulin.
Here is a breakdown of the various diabetes medications.
Oral Diabetes Medications
- Sulfonylureas – A group of medications that works by increasing the release of insulin from the pancreas. Common sulfonylureas include:
- DiaBeta
- Glynase
- Amaryl
- Diabinese
- Glucotrol
- Tolinase
- Tolbutamide
- Biguanides – A class of medicines that works by reducing the production of glucose during digestion. Metformin is the only biguanide available. Common brand names include:
- Glucophage
- Glumetza
- Fortamet
- Riomet
- Thiazolidinediones – This is a group of medicines that improves the way insulin works. Common thiazolidinediones include:
- Actos
- Avandia
- Alpha-glucosidase Inhibitors – This is a class of drugs designed to delay the absorption of carbohydrates in the intestines, lowering postprandial blood sugar levels. Common brand name drugs of this class include:
- Precose
- Glyset
- Meglitinide – These are medications that work by triggering the production of insulin. Common meglitinides include:
- Prandin
- Starlix
- DPP-4 Inhibitors – This is a class of drugs that promotes the pancreas to release more insulin after meals and lower the amount of glucose produced by the liver. Common medications include:
- SGLT2 Inhibitors – This group of medications works by preventing the kidneys from reabsorbing glucose back into the bloodstream. Common medications include:
- Bile Acid Sequestrant – This class of drugs can improve glycemic control and lower bad cholesterol (LDL). Common medications include:
- Dopamine Agonist – These drugs can help reduce the amount of glucose released by the liver. Common medications of dopamine agonist include:
Non-Insulin Injectable Medications for Type 2 Diabetes
- Amylin Analogs – Medications in this class are administered subcutaneously and act similarly to the physiological amylin. Amylin is an amino acid polypeptide hormone that is released with insulin to help with postprandial glucose control. The most common medication of amylin analogs include:
- GLP-1 Agonists – This class of drugs mimics the hormone known as glucagon-like peptide 1, which stimulates the pancreas to secrete more insulin. GLP-1 agonists also promote weight loss, which is important for those with type 2 diabetes. Common medications of this drug class include:
- Betta
- Adlyxin
Using insulin pumps and continuous glucose monitors to manage diabetes
One common treatment method, particularly for type 1 diabetes, is the use of insulin pumps and continuous glucose monitors.
Insulin pumps are small devices that mimic how the pancreas works. They can be programmed to deliver a continuous drip of insulin, replacing the need for long-acting insulin.
Patients can also easily administer boluses for any meals or corrections they need. These devices allow for greater convenience and better-controlled blood sugar levels.
The two types of insulin pumps available are:
- Traditional insulin pumps contain a reservoir of insulin, a pumping mechanism, and attaches to the body via a tube and infusion set. The device itself allows you to program the settings for specific dosages.
- Insulin patch pumps are small pods worn directly on the body. They also contain a reservoir, pumping mechanism, and cannula inside the pod. They are controlled wirelessly with a programmable phone-like device.
Despite the convenience and ease of use that insulin pumps provide, some may still prefer multiple daily injections. See our blog on Insulin Pumps vs Injections.
Continuous glucose monitors (CGMs) are devices placed directly on your body and continuously monitor your glucose levels. However, CGMs measure the glucose in the interstitial fluid and not the blood. Therefore, there is often a 10–15-minute delay compared to your real blood sugar reading.
CGMs help patients fully understand how different factors affect their blood sugar levels. In turn, they can better control their blood sugar and live a healthier life.
Common continuous glucose monitors on the market include:
- Freestyle Libre
- Dexcom
- Medtronic Guardian
The manufacturers of insulin pumps and CGMs have started to work together in recent years and are working towards creating an artificial pancreas. This would essentially allow the insulin pump to administer insulin based on the CGM readings without the patient having to make adjustments.
Conclusion
Diabetes is not an easy condition to deal with, but with proper management, you can live a healthy life. So, we hope this article has given you a better understanding of what diabetes is and how you can manage it.
We understand that affording your diabetes medication can be difficult and even impossible for some. The cost of prescription drugs has been on the rise, which has added a lot of stress on many individuals.
Prescription Hope exists because of this problem in the United States. The advocates here work directly with pharmaceutical manufacturers to provide patients with their needed medication at a set, affordable cost through Prescription Hope’s medication access program. Enroll with us and start saving money .

