Everything You Should Know About Injecting Insulin – A Guide
Posted by Prescription Hope - See Editorial Guidelines (Last Updated On: Fri Apr 21 2023)
Anyone who has type 1 diabetes and some patients with type 2 diabetes will require insulin therapy. Injecting insulin for some individuals may be a daunting task, especially if you are newly diagnosed with diabetes. Before discussing all of the details around injecting insulin, here is a quick summary of what you should know. What you should know about injecting insulin: You can inject insulin in three different ways – a syringe, a pen, or a pump. The method by which you inject insulin highly depends on your personal preference. However, there is a right way to inject insulin, and injecting insulin improperly may result in uncontrolled blood sugars. In this article, we’ll discuss everything you need to know about injecting insulin.
Ways Insulin Can be Administered
 Injecting insulin is the most common way of administering the medication. However, there is an insulin that can be inhaled. It is not as popular, but individuals may benefit from inhaling insulin if they have injection site reactions often. The only inhaled insulin on the market is Afrezza.
There are three ways that an individual can inject insulin. They consist of using syringes with a vial, an insulin pen, or an insulin pump.
The way one decides to inject insulin is highly dependent on personal preference and lifestyle factors. Your doctor may make a suggestion based on your current blood sugar control. However, some individuals find pumps to be the most beneficial for them, whereas some dislike having an insulin pump attached to their body.
It is important to note that when you inject insulin using a syringe or a pen, you should hold the needle in place for 10 seconds after fulling injecting the dose. This ensures that you receive the full dose needed.
Regardless of the method for injecting insulin that you use, your doctor should provide you with proper training on how to inject.
Injecting insulin is the most common way of administering the medication. However, there is an insulin that can be inhaled. It is not as popular, but individuals may benefit from inhaling insulin if they have injection site reactions often. The only inhaled insulin on the market is Afrezza.
There are three ways that an individual can inject insulin. They consist of using syringes with a vial, an insulin pen, or an insulin pump.
The way one decides to inject insulin is highly dependent on personal preference and lifestyle factors. Your doctor may make a suggestion based on your current blood sugar control. However, some individuals find pumps to be the most beneficial for them, whereas some dislike having an insulin pump attached to their body.
It is important to note that when you inject insulin using a syringe or a pen, you should hold the needle in place for 10 seconds after fulling injecting the dose. This ensures that you receive the full dose needed.
Regardless of the method for injecting insulin that you use, your doctor should provide you with proper training on how to inject.
Injecting Insulin with a Syringe
An insulin syringe has four parts, which consist of the cap, the needle, a barrel, and a plunger. The cap is simply used to cover the needle for protection. The barrel is the portion of the syringe that holds the insulin once it is taken from a vial. The barrel of the syringe has markings on it to measure the dose of insulin. The plunger component fits perfectly inside the barrel of the syringe. It slides up and down to draw insulin into the barrel and to push insulin out through the needle. A rubber seal is at the bottom of the plunger to prevent insulin from leaking out of the syringe. The table below is a size chart for insulin syringes. You should use the smallest syringe size possible for the dose you need.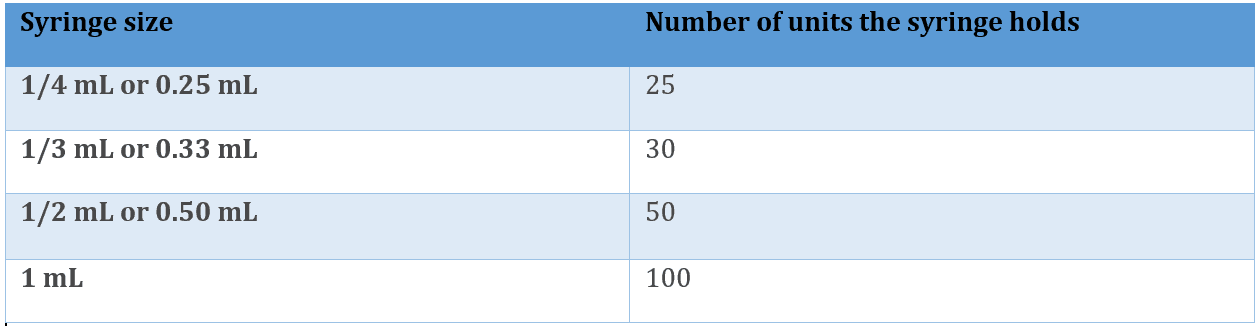
Injecting Insulin with a Pen
An insulin pen has the appearance of a large writing pen. Most insulin pens contain 300 units of insulin. At one end of the pen is a dial that is used to measure your dose by either 1 unit or ½ unit increments. At the other end of the insulin pen is a place where you have to screw on a small pen needle, which comes as a separate component. Once you have the needle placed on the pen and have dialed up your correct dose, you then push down on the plunger. After you have fully injected the insulin, recap the needle, and unscrew it from the pen. Dispose of the capped needle into a sharps container and place the cover back on the insulin pen.Injecting Insulin with Pumps
Most insulin pumps generally work in a very similar way when it comes to injecting insulin. The specifics and look of the insulin pump will vary, depending on which one you use. A pump differs from the other two methods of injecting, as it provides a continuous delivery of short-acting insulin. The pump also replaces the need for multiple injections every day. Most insulin pump infusion sites need to be changed every 48-72 hours. When injecting insulin with an insulin pump, you first have to fill the pump cartridge or reservoir. This is done by using a syringe and vial. There is tubing that connects to the reservoir, and insulin travels through the tubing and into the subcutaneous tissue. The tubing may also be called a cannula.Preparing Your Injection of Insulin
Diabetes is, perhaps, the only condition where the patient has to self-dose and administer their medication. So, when preparing your dose of insulin, you must ensure that you are giving yourself the correct amount of insulin based on your carb consumption and your current blood sugar reading. Therefore, you must check your blood sugar often and before giving yourself insulin. When giving a mealtime dose of insulin, you should be counting carbs. This means utilizing your insulin to carb ratio to determine your full dose.
You should not give yourself a mealtime insulin injection if you are eating to correct hypoglycemia.
When preparing a correction dose, you must know what your correction factor is. A correction factor is how much one unit of rapid-acting insulin will reduce your blood sugar. A correction bolus should never be given if your blood sugar reading is at or below your target range. If a correction is needed before a meal, then your correction dose should be added to your meal bolus.
There are times where you should not prepare an injection of insulin for a correction. These times include if it has been less than three hours since your last meal, less than one hour since exercise, or right before going to bed unless otherwise specified by your doctor.
Therefore, you must check your blood sugar often and before giving yourself insulin. When giving a mealtime dose of insulin, you should be counting carbs. This means utilizing your insulin to carb ratio to determine your full dose.
You should not give yourself a mealtime insulin injection if you are eating to correct hypoglycemia.
When preparing a correction dose, you must know what your correction factor is. A correction factor is how much one unit of rapid-acting insulin will reduce your blood sugar. A correction bolus should never be given if your blood sugar reading is at or below your target range. If a correction is needed before a meal, then your correction dose should be added to your meal bolus.
There are times where you should not prepare an injection of insulin for a correction. These times include if it has been less than three hours since your last meal, less than one hour since exercise, or right before going to bed unless otherwise specified by your doctor.

