Insulin Pump vs. Injections – What’s the Difference, Which is Better
Posted by Prescription Hope - See Editorial Guidelines (Last Updated On: Mon Apr 24 2023)
Everyone that has type 1 diabetes and some that have type 2 diabetes will need insulin for them to control blood sugar levels. So, this provides the need for the discussion of insulin pump vs. injections.

Those with diabetes and in need of insulin will, at some point, have to decide between an insulin pump or insulin injections. There are pros and cons to both options, which can vary from individual to individual.
After discussing the pros and cons of insulin pump vs. injections, I will give my personal opinion as someone that has type 1 diabetes and has used both forms of insulin delivery.
Insulin Pump vs. Injections – The Differences
Insulin pumps can come in a variety of different forms depending on the manufacturer of the pump. However, the concept of each insulin pump remains the same.
Essentially, an insulin pump is a small computerized device that continuously delivers insulin every hour (basal rate), and you can deliver a bolus by merely plugging in the amount of carbs consumed. An insulin pump is typically about the size of a small deck of cards. It will either attach directly to the body via an adhesive (i.e. Omnipod), or the device connects to a cannula that is inserted underneath the skin opposite the device.
Daily insulin injections, on the other hand, are typically delivered via insulin pens. This is precisely what it sounds like. It is a pen looking device that contains insulin. A small needle is placed on one end of the pen, and a dial, used to measure the dose, is at the other end of the pen. Once the needle is screwed on and the dosage is set on the dial, you then inject the insulin.
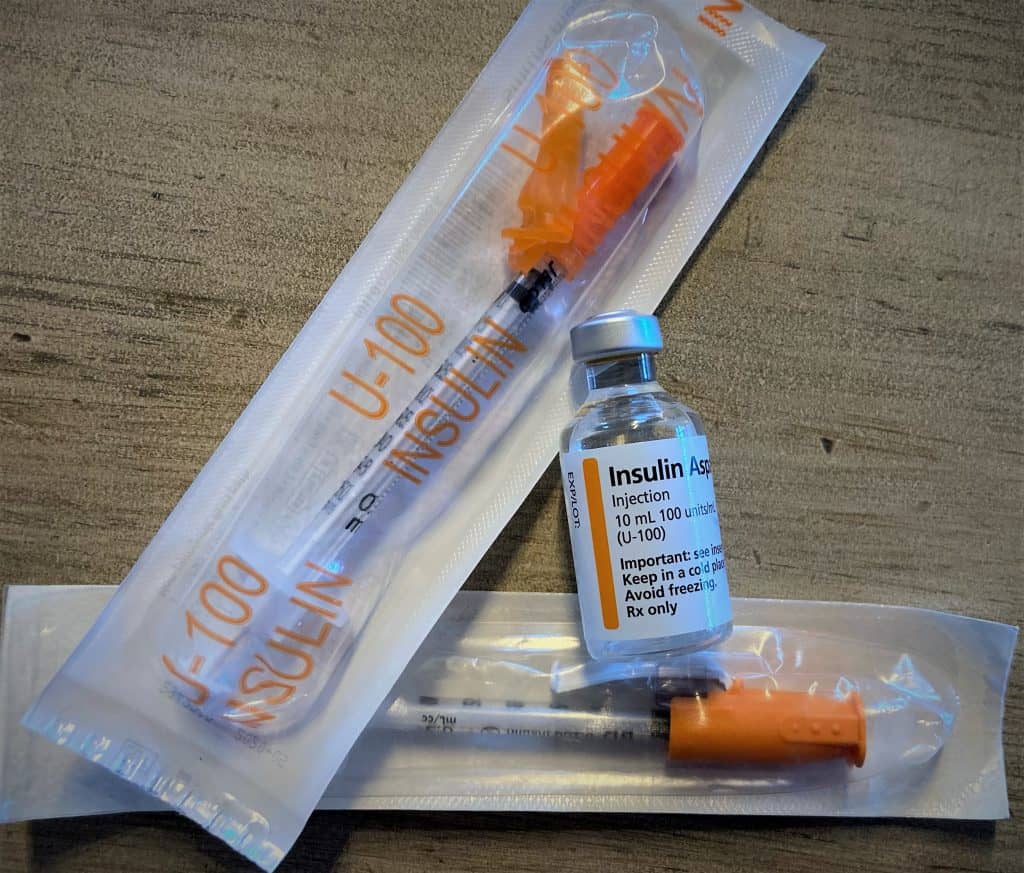
Daily injections can also be done via a syringe and vial. You use the syringe to take the needed amount of insulin out of the vial, then inject it.
Daily insulin injections are delivered at every meal, whenever a correction is needed, and an injection of long-acting insulin is typically required once a day.
Now that we have a basic understanding of how each works let’s get into the positives and negatives of insulin pumps and injections.
Insulin Pump Pros and Cons

Many individuals and doctors find the insulin pump to be beneficial as it can help individuals find better control of their blood sugars. Patients using insulin pump therapy can sometimes find more freedom through the pump vs. injections.
Some insulin pumps are used with a continuous glucose monitor (CGM) to provide a closed-loop system. This means the patient can worry less, as the pump and CGM work together to ensure stable glucose levels without requiring much manual dosing.
Pros
- Dosages are delivered easily throughout the day
- Basal rate is automatic and constant
- Insulin pump infusion sets can be changed every few days
- Corrections are easily made
- You can suspend basal rate making it easy to adjust dosage during exercise
- Pumps can be programmed to deliver different doses of insulin automatically at specific times
Cons
- Changing out infusion sites can be a process
- Pump problems can occur such as a kink in the tubing or air bubbles in the insulin cartridge
- Takes longer to learn the ins and outs of an insulin pump
- Pump equipment and accessories can be pricey
- It can be uncomfortable to wear all-day
- Sometimes the pump can be visible making it socially uncomfortable for some
Daily Injection Pros and Cons
Not everyone finds an insulin pump to be beneficial. There might be a few different reasons for this, whether its finances or they feel uncomfortable wearing a pump. Depending on the individual, they may switch back to insulin injections after being on a pump for a while.
Pros
- Simple to perform injection
- Not as expensive
- Always have background insulin working (long-acting insulin injection)
- There’s no risk of being away from home and having a pump failure or mechanical issue
- Nothing is attached to the body, nor is there any tubing involved
- Injection pens can be used discretely
Cons
- Multiple injections a day
- You cannot change the basal rate once the long-acting insulin has been injected (have to wait 24 hours before making changes to the dose)
- The background insulin needs to be administered at the same time every day
- Administering the insulin shot in public can feel socially uncomfortable
My Experiences
To provide myself with some credibility here, let me briefly describe my experience with the use of an insulin pump vs. injections. I was diagnosed with type 1 diabetes in November of 2013. While in the hospital and being treated for DKA, I learned to give myself an insulin injection via syringes and vials. For the first year after my diagnosis, I used insulin pens, giving myself about 5-8 injections a day. Since then, I have been on an insulin pump. I have only used one type of insulin pump, so my experience with the pump may be biased to an extent.
If you are looking for me to tell you what you should do, you won’t find that here. However, I will give you some insight into my experiences, which should give you an idea of what might be best for you. We always recommend speaking to your doctor about what would be best for you.
While I was performing daily injections, via insulin pens, I hated it. I think that I hated it so much because I was still learning to adjust to the diabetic lifestyle. So, after a year of continuously sticking myself with needles multiple times a day, I was thrilled to get an insulin pump.
The insulin pump I got and have been on is a tubeless patch pump that has to be changed every three days. At first, it was amazing. As time went on, though, I realized it wasn’t all sunshine and rainbows with the insulin pump. There are still difficulties to navigate.
There have been multiple times where the pump failed, whether the adhesive wore out too quickly, the cannula kinked, or a mechanical failure occurred. This has happened in the middle of the night, during social events, work, and school, which is extremely inconvenient.
There is no worse feeling than going out to eat or out with friends, and you hear your pump beeping telling you that insulin delivery has stopped. There are times where you don’t have a replacement pump with you, and you have to improvise.
During these times, I have to choose to either not eat or drink anything other than water until I can get back home, or I head home right away to replace the pump. As I experience these times, I always think to myself, “this wouldn’t be happening if I just went back to daily injections.”
However, I also realize that going back to daily injections would mean that I would have to be way more disciplined with my diet and with my dosing. With the insulin pump, I can be a little more relaxed with the times I’m eating and can have many smaller meals throughout the day, which is what I prefer. With injections, I have to give myself a shot with every small snack, which is tedious and annoying.
I am also very much into fitness and working out, so having an insulin pump attached to my body can feel inconvenient at times. The pump has never prevented me from working out or from performing various lifts and exercises. However, it can feel uncomfortable.
Though I am still currently using an insulin pump, I continuously debate about going back to daily injections. It could save me money, and I wouldn’t have to worry about ripping my insulin pump off every day. However, I know that if I go back to daily injections, I will miss the convenience of the pump and the freedom it gives me.
Needless to say, I have my opinions about both insulin delivery methods. There is no easy way to dealing with diabetes, and you have to find what works best for you and what you are most comfortable with.
I see myself utilizing both insulin delivery methods in the future. Perhaps wearing the pump for a full month and taking a break for a few weeks by using insulin injections.
Taking a Break from Insulin Pump
If you have been using an insulin pump for some time, you may be getting tired of having it attached to your body. This may warrant a time to take a break from the insulin pump just to keep your sanity.
When taking a break from the insulin pump, there are some things you need to consider first to ensure your safety and health. Here are some tips to help you with taking a break from your insulin pump.
Make sure you have all the necessary supplies
The obvious first step here is you need to make sure you have everything you need to take a brief break from insulin pump therapy. This includes both short-acting and long-acting insulin pens and pen needles. Some insulin pens come with half-unit dosing increments, which may be helpful in getting better control of your blood sugar if you have been used to using a pump.
Adjust your basal dose
To calculate your basal dose for daily injections, find the sum total of your daily basal rate on your pump. For example, your basal rate may be.85 units every hour for the entire day. This would total out to 20.4 units for the entire day. So, your starting long-acting insulin dose should be about 20 units per day in this case. You can then make adjustments to the dose based on your blood sugar readings. You should not make any major or rapid adjustments to your insulin dosages without first consulting your doctor.
Don’t skip meals
When taking a break from your insulin pump, it is important to remember that once you inject your long-acting insulin, there is no stopping it. With your pump, you can suspend your insulin if you were skipping a meal or working out. You cannot do that on daily injections. So, it is important to monitor your blood sugar carefully and avoid skipping any meals to prevent low blood sugars from occurring.
Use a bolus calculator
If you have been using an insulin pump, then chances are that you have not had to do a lot of math to calculate your bolus dosages. The pump will take into account your insulin to carb ratio and your correction to calculate your total bolus. If you have not done this manually in a while it can be difficult to properly calculate your short-acting insulin dose. Therefore, it may prove to be helpful to use a bolus calculator when taking a break from your insulin pump.
Conclusion
I hope that this article has given you some insights into the use of an insulin pump vs. injections. Finding the insulin delivery method that works for you can be difficult. But adding in the financial burden of purchasing insulin and other diabetes supplies makes it even more difficult.
Prescription Hope is here to help you afford your diabetes medications or any other prescription medications. We work with 180 pharmaceutical companies and have over 1500 brand-name medications in our system. Prescription Hope is a medication access service-based company that provides you with the medication you need for just $60.00 a month through Prescription Hope’s medication access service for each medication. Enroll with us to find out if you are eligible.

