What is Time in Range and Does it Matter? A Diabetes Metric
Posted by Prescription Hope - See Editorial Guidelines (Last Updated On: Fri Apr 21 2023)
Time in range is a metric used by those contending with diabetes and doctors that specialize in diabetes. It is used to determine how controlled one’s blood sugar levels are. Understanding this metric is crucial, as it gives you and your doctor a better understanding of how well your diabetes condition is controlled.
So, we will discuss what time in range is and why it’s important. First, here is a summary to give you a quick answer.
What is Time in Range? Time in range, sometimes abbreviated as T.I.R, refers to the percent of time a person’s blood glucose levels are within a specified target range. It captures an overall depiction of one’s control over their diabetes condition. The lower the percent of time in range, the less controlled their condition is. You need at least two weeks’ worth of blood glucose information to determine an accurate time in range.
Now that you have the quick answer, let’s get into the details.
What is Time in Range?
Time in range is the amount of time a person’s blood glucose is within a specified target range. It is measured as a percent, but the percent represents time.
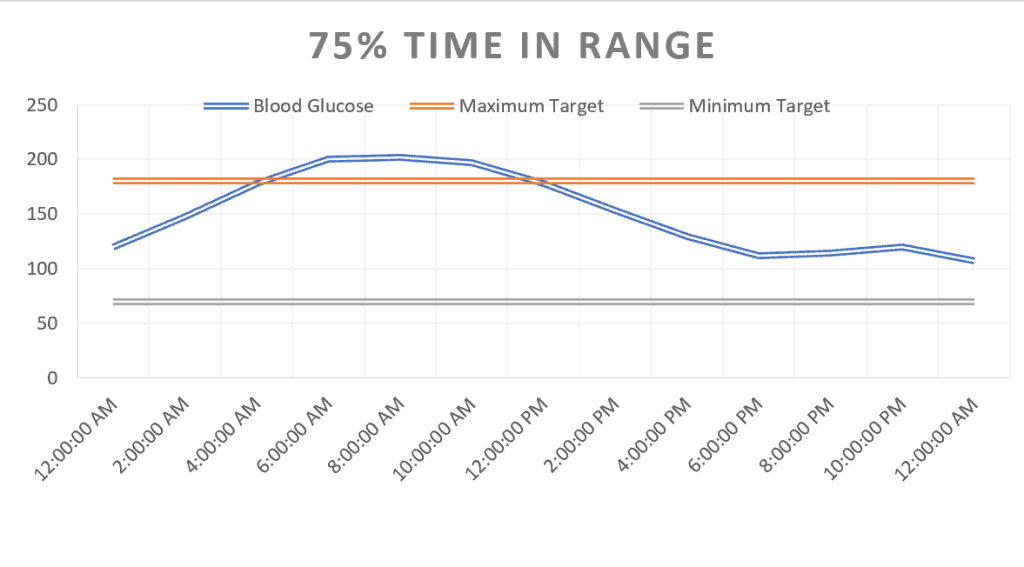
So, for example, if a person’s time in range is 75%, then their blood sugar levels were within the target range for 18 hours of the day and out of range 6 hours of the day.
The specific target range will vary slightly among individuals. Many certified diabetes educators will recommend a target of 70-180 mg/dL. Staying above 70 mg/dL keeps you from having dangerous hypoglycemic events. Striving to stay below 180 mg/dL will keep you from experiencing dehydration due to sugar spilling into the urine.
Most health professionals want their patients to spend as little time as possible below their target range. Anything more than 5% below their target range means they are having too many low blood sugar events, which can be dangerous.
Why is Time in Range Important?
Time in range is crucial because you could have three different people that all have the same A1C results but different time in range results. It is also important because those with diabetes that have a greater time in range will have a greater quality of life. Those that have blood sugars that are largely out of range will experience lower energy levels and poor moods.
An A1C is the average blood glucose level for the past 3 months. This is one test used to determine how well one’s diabetes condition is being managed. However, doctors will often compare the A1C test results with other information, such as time in range results.
So, if two patients have the same A1C, this does not mean they both have their condition well managed. For example, they may have an A1C of 6.5%, which translates to an average blood sugar of about 140 mg/dL. Patient one may then have a time in range of 75% and patient two may have a time in range of 50%. Therefore, patient two is having greater fluctuations in their blood sugar levels, experiencing more high and low blood sugar readings that average out to about 140 mg/dL. On the other hand, patient one is keeping their blood sugar levels fairly steady, preventing large spikes and severe lows. Thus, patient one is managing their condition much better than the other patient.
The time in range data is important for helping one understand how various aspects of one’s life affect blood sugar control. For example, the data will allow you to see how different foods and exercise affect your blood sugar levels.
Relationship Between Time in Range Glucose and Complications
Researchers believe that long-term time in range is an accurate determining factor for if a person will experience complications. Therefore, there is a relationship between time in range and diabetes complications, which may include diabetic retinopathy and kidney disease.
High blood sugar levels have a direct impact on the function of cells and various organs. The higher one’s blood sugar goes, the more damage that is likely to occur to the eyes, kidneys, and nerves.
So, to sum it up the relationship between time in range and complications, the higher the time in range percentage, the lower the risk of having complications.
How to Measure Time in Range
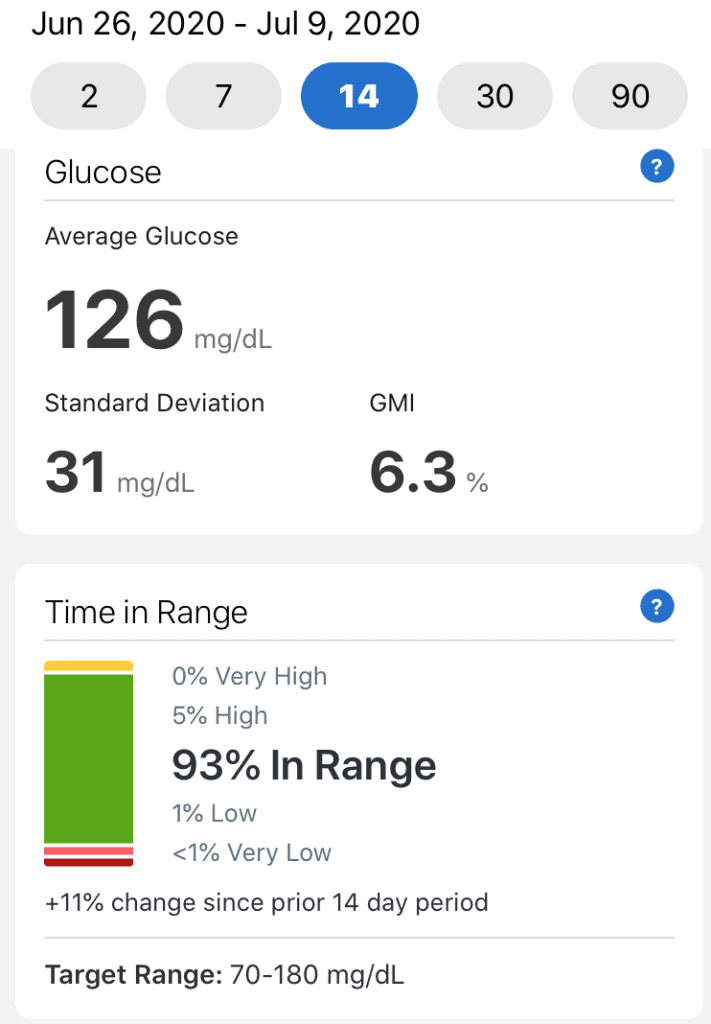
The most accurate way to measure time in range is to use a continuous glucose monitor (CGM). A CGM continuously measures your blood sugar levels every five minutes, so it will give you the most information for determining time in range. Most CGMs have software that will automatically calculate the data.
However, not everyone has a CGM, and they can be pricey. So, a normal blood glucose meter can be used, but it will not provide the most accurate information. When using a glucose meter, you will get a better idea of what your time in range is with the more fingersticks that you take.
There are apps and other software available that allow you to upload the readings from your meter directly. Many of these apps will take the data from the readings and automatically calculate time in range.
If you do not have an app or a glucose meter that will upload the data, then you can calculate your time in range using the equation below.
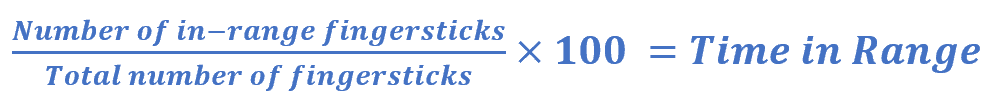
Typically, it is recommended to have at least two weeks’ worth of data to measure your time in range.
Improve Your Time in Range
The first step in improving your time in range is understanding where your blood sugar levels currently stand. You have to know the trends of your blood sugar levels before you can know what steps you can take to improve your condition.
To do this, it is recommended to use a CGM. A CGM is extremely beneficial for those struggling to control their blood sugar levels. It will allow one to see how their blood sugar reacts to various factors. If a CGM is not accessible for you, then consider performing more fingersticks to check your glucose more often.
After understanding how your blood sugar levels are currently reacting to various factors, such as certain foods, take steps to mitigate large fluctuations in blood sugar. So, if you are noticing large spikes in blood sugar after each meal, then you may want to consider lowering your carbohydrate intake at each meal. If you are experiencing low blood sugar levels during exercise, then have a small snack 20 minutes prior to exercising.
When your blood sugar is out of range, then make proper corrections. This means you need to know what your correction dose is for high blood sugar levels. For example, it could be that 1-unit insulin lowers your blood sugar by 30 mg/dL. So, if your blood sugar is 200 mg/dL several hours after eating and you want to get down to 140 mg/dL, then you may inject 2 units of insulin. Your doctor will work with you to determine your correction factor.
Identify which days you have the most time in range. Take notes of what you did and what you ate those days, along with the amount of insulin administered. Strive to replicate the actions taken that day to continue keeping your glucose in range.
Finally, create a schedule and a routine. I have found that my blood sugars become less controlled when I am not in my typical routine, such as when I travel. Sleep patterns can be disrupted, the times I eat change, what I eat changes, and I don’t get the normal exercise I’m used to. All of this makes it difficult to keep blood sugars in range. So, build a routine so that you can be as consistent as possible.
Conclusion
We hope that you can gain better control over your diabetes condition by gaining more insight into the time in range metric. If you are struggling to keep your blood glucose levels in range, then consult your doctor.
If you are having trouble affording your insulin or other medication, then Prescription Hope can help. We work directly with pharmaceutical companies to help patients obtain their medicine at a set, affordable cost. Enroll with us and pay just $60.00 a month through Prescription Hope’s medication access service for each of your medications through Prescription Hope’s medication service.
ENROLL



