Diabetes and Heat, How Heat Affects You and Insulin, What to Do
Posted by Prescription Hope - See Editorial Guidelines (Last Updated On: Tue Apr 25 2023)
People with both type 1 and type 2 diabetes go through several blood sugar patterns during summer and it’s essential for them to be monitored to prevent a situation of high/low blood sugar levels. Diabetes and heat can be a dangerous combination if not monitored carefully. This article will provide you with a complete guide on how heat affects diabetes and how to manage it.
How Heat Affects Diabetes? Hot days, high temperatures and sunburn can easily cause dehydration, which increases blood sugar levels due to glucose concentration. Heat also burns more calories and glucose, causing low blood sugar. Even diabetes medicines and aids lose their effectiveness in treating diabetes when exposed to heat.
When extreme heat is reported in the news, it’s the diabetic patients who feel the heat more than those who do not have diabetes.
For easy identification, if you’re a diabetic patient you may sweat profusely during a hot summer. This is because diabetes has a strong connection with heat.
Heat and High Blood Sugar Levels

The first thing we are faced with when it comes to the combination of diabetes and heat is dehydration. We all know during summer we dehydrate more. It doesn’t matter whether it’s hot and humid or hot and dry, mild-to-severe, we all easily dehydrate during hot weather.
For those not aware, 60 percent of our body weight is water, 75 percent of our muscle weight is water and even 85 percent of our brain is water.
Likewise, water is a crucial element for the effective functioning of our body. What happens when you dehydrate is that the glucose levels in your bloodstream become a lot more concentrated.
This concentration of glucose happens due to reducing water levels in the body. This is because when you dehydrate there’s an inadequate amount of fluid within your tissues and bloodstream to keep it diluted.
When glucose concentrates, it increases your blood sugar levels. And this, in turn, will cause you to urinate more, which has the effect of causing further dehydration, yet again spiking your blood sugar levels.
Dehydration and the high concentration of glucose can, therefore, spike your blood sugar levels by 50mg/dL – or over 200 mg/dL. So just a small amount of dehydration daily can increase or change your insulin need more than on other days.
Similarly, when you don’t eat anything or drink anything during summer, like spending all afternoon in the sun in 95-degree heat, you would expect your blood sugar to reduce. But in contrast, the added dehydration causes your blood sugar to spike rapidly.
Again, even if it’s not that hot outside, the combination of humidity and heat can spike your blood sugar. This is because when you sweat, naturally your sweat evaporates and cools you down, causing a reduction in the level of dehydration. But in high humidity (high moisture in the air) it’s hard for you to stay cool because the sweat doesn’t evaporate.
So, when it’s hot and humid, you may sweat more causing more and more dehydration and spiking up your blood sugar level rapidly.
Insulin, Heat and the Heat Index

The first thing to remember with diabetes and heat is that high temperatures can affect the way how your body uses insulin.
You might first have to test how the insulin actually works for your body and adjust your insulin dose accordingly.
Adjusting insulin dose should be backed up with a proper diet, meaning a greater intake of fluid and other food that contains minerals to make sure you’re properly hydrated at all times.
In addition to these, it’s also a good idea to check the heat index when the temperature soars.
The heat index is a measurement that combines heat and humidity. It’s always good to take steps to stay cool when the temperature reaches anything like 80°F (26°C).
The heat index can even go up to 15°F higher in full sunlight, so make sure you stick to more shaded areas when the weather warms up.
Humidity has a huge influence on temperature, for example, when the temperature is 90°F (32°C), a high humidity index could make it feel more like 105°F (40°C).
Heat, Sunburns and Blood Sugar Levels
One major complication that occurs between diabetes and heat is sunburn. It is one of the most obvious things we experience during the summer. It is often overlooked, but sunburns do affect blood sugar levels.
What happens when you’re sunburnt is that there’s intense damage on your skin, which is stressful.
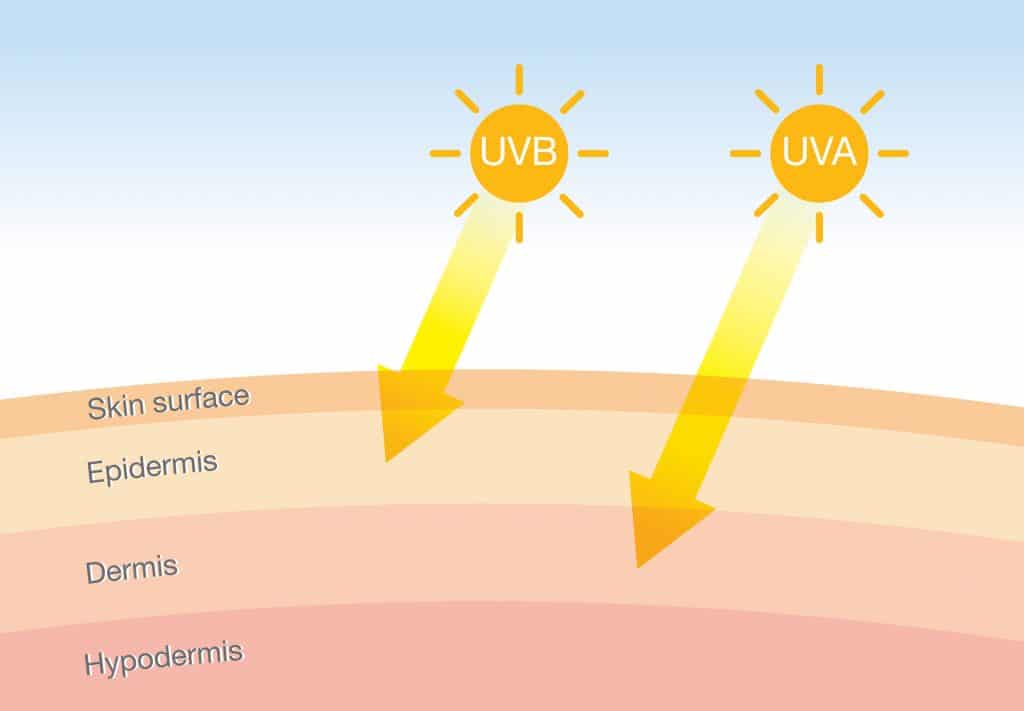
A physical injury will always be stressful on the body. The same applies to a sunburn. A sunburn is stressful for the body and creates a great deal of inflammation.
So, the body will have to adjust and manage to overcome the inflammation and heal. The healing process comes with other hormones including cortisol.
These hormones are those that help manage and heal any inflammation. Although it may sound like a normal healing process for diabetic patients – it’s not.
For a diabetic patient, this process results in temporary insulin resistance and higher blood sugar levels.
Thankfully these sunburns don’t last for more than a couple of days. If you have a severe sunburn then, of course, the healing process will be slower and the effect of it on your blood sugar levels could be even higher.
In a situation like this, it’s better to consult directly with your healthcare team. Ask them to investigate an increase in your background insulin needs to keep your blood sugar levels in the healthy range.
This will also give your body the required ability to heal the sunburn quicker too.
How to Manage Sunburn with Diabetes
It’s important to remember the concept we outlined before, that sunburn causes dehydration leading to a spike in your blood sugar levels.
This is because sunburns increase your body temperature leading to dehydration. So, to appropriately and effectively avoid the effects of a bad sunburn. You should always keep yourself hydrated.
When you’re outside for even a short period on a hot day, check your blood sugar levels regularly.
But it’s not advisable to simply anticipate that you’ll be sunburnt or dehydrated on your day out…and take insulin prior. Doing this is highly risky because any insulin that’s taken before high blood sugar levels can easily lead to hypoglycemia.
Only when you feel any mild to moderate effects of dehydration due to sunburn you should seek to find shade and take in a good amount of water.
Here you could also take a carefully calculated dose of insulin. You might be tempted to take a large dose due to the heat, but this can lead to severe plummeting of low blood sugar levels.
And of course, wear more sunscreen too if you know you’re about to spend the time outdoors during hot weather, this will keep your skin moist and protect it from being dried out. This will, in turn, reduce any potential dehydration and avoid any blood sugar spikes.
Heat and Low Blood Sugar Levels

Here what happens is the body burns glucose far more quickly than it does on a less hot day. Like a slow and steady walk, during hot days your body burns more glucose trying to keep your body cool.
Especially exercising during a hot day can easily reduce your blood sugar levels. Even if you do everything possible to prevent low blood sugar during exercises, a hot day can easily result in low blood sugar.
Some research has shown that your body works harder to stay warm in cold weather compared to cooling down in hot weather. But despite this, during hot days, there is an increased caloric burn that results in burning more glucose. So, a low blood sugar level becomes highly likely.
How to Manage Diabetes and Heat
Predicting exactly what leads to low blood sugar on a hot day and avoiding them can be difficult.
This is because many factors affect low blood sugar levels. From what you ate last, to what insulin dosage is prescribed by your doctor, plus your activity level compared to hydration level, and even the current blood sugar level affects a condition of low blood sugar.
And in addition to these, the menstrual cycle in a woman could lead to an entirely different blood sugar level or responses every other day of the menstrual period.
The best thing you can do in this circumstance is to be prepared. Check your blood sugar levels regularly. Keep fast-acting carbohydrates within reach at all times. Especially when you’re exercising make sure you have candies or fruit juices handy.
Also, make sure you stay hydrated at all times – which is naturally what we’re all told is one of the most obvious things we should do during summer or hot days – but even more so for diabetics.
Apart from these, there are other diabetes complications affecting your sweat glands. Damages to blood vessels and nerves are also potential complications.
This will affect the sweat glands in a way that your body can’t cool down effectively or efficiently enough. In such cases, a diabetic patient may be exposed to greater risks during hot days or in summer.
In patients with these conditions, heat can easily lead to heat exhaustion and heat stroke, which as you may know are medical emergencies.
While the above explanation shows how heat affects blood sugar levels. There are other factors involved that can affect diabetics.
Even the insulin, insulin pumps, or glucometers we use can be affected by heat. Thereby, reducing the overall response or effectiveness it has to provide to control your blood sugar levels.
Heat, Insulin and Insulin Equipment Trouble
The ideal temperature for insulin equipment and insulin solution is between 36 to 46 degrees Fahrenheit.
When your insulin is exposed to temperatures more than this recommended amount, or even exposed to heat for a long period of time – the insulin will breakdown.
This breakdown of insulin can be very severe, where the insulin will become essentially useless for managing your blood sugar levels.
The ideal temperature for insulin equipment and insulin solution
is between 36 to 46 degrees Fahrenheit
The breakdown can occur in a very short time. For example, an 80-degree temperature in summer and 20 degrees in the winter can easily breakdown the insulin – perhaps at a glance.
And in case you weren’t aware, insulin also begins to breakdown the moment you open a vial or pen.
This is why it’s generally suggested that you use any opened insulin within 28 days. But during hot weather, the usability of insulin could be reduced to far fewer days – depending on the temperature.
If you are wearing an insulin pump, beware of your use of sunscreen. As mentioned above in this article, it is important that you wear sunscreen during hot days. However, some insulin pumps, such as the Omnipod, may crack or become defective if certain sunscreens have contact them. Talk to the manufacturer of your insulin pump about this.
How to Manage
The standard temperature for insulin is generally recommended to remain at room temperature, which is warmer than 46 degrees.
In which case, the insulin can be safe when it’s in your home somewhere on the shelf or even when you’re walking around with it in your purse or bag.
But your insulin may be at risk in hot temperatures in certain situations – such as.
- When insulin is left in your car on a hot day with windows closed or without the AC on.
- Wearing the insulin pump too tight or attached to the skin that the body heat easily penetrates to the pump. Especially when exercising or walking out in hot weather.
- Leaving the insulin almost directly under the sun on an outdoor picnic table on a very hot day.
- Packing insulin in your suitcase during air travel.
- Leaving insulin in a bag or purse under shade on a very hot day.
So, you ideally need to think about protecting your insulin from these or similar kinds of situations.
Also, you can make really good use of coolers, ice packs and Frio-packs – a pack that needs zero refrigeration to protect your insulin from extreme temperatures. Here’s the info on whether you can freeze your meds.
Or you could make use of apps like MedAngel, which alerts you when you’re in an environment with temperatures that are unsafe for your medications.
Special Tips for Managing Diabetes and Heat
- First, always drink plenty of water to keep yourself hydrated at all times – even if you’re not thirsty.
- Pick drinks wisely – avoid alcohol and drinks containing caffeine. Drinks like coffee and energy or sports drinks can lead to greater water loss. This will spike up your blood glucose levels more than dehydration.
- Wear loose, lightweight, comfortable and light-colored clothes that will reflect heat rather than dark colors that absorb heat.
- Always wear sunscreen when you’re spending time outdoors.
- Wear footwear at all times – don’t walk barefoot.
- Use an air conditioner or make sure you stay in an air-conditioned location whenever possible. Often, in extreme heat, a fan is not enough to cool you.
- In hot days or high temperatures, people are at risk of both high and low glucose levels. So, you may need to adjust your insulin dosage appropriately. Ask your doctor regarding this.
To Finish…
We hope this has been helpful in understanding how heat can affect not only you as someone who may have diabetes, but also the equipment and insulin supplies you have.
As always, these are guidelines only, if you’re in any doubt then consult your doctor for advice.
If you’re having trouble affording any of the medications you’ve been prescribed, contact us, or visit the enrollment page to create an account and fill out an application to start saving.
ENROLL



