Are you experiencing digestive problems and wondering why? If you have diabetes, then you may be suffering from diabetic gastroparesis.
In this article, we will discuss what diabetic gastroparesis is, including the symptoms, causes, and treatment options. First, let’s get started with a quick takeaway answer.
Diabetic Gastroparesis: Diabetic gastroparesis refers to a particular digestive problem that is directly caused by high blood sugar associated with diabetes. This condition disrupts the contraction in the stomach responsible for moving food through the digestive system. This can lead to symptoms such as nausea, heartburn, bloating, and loss of appetite.
With this quick answer in mind, let’s cover the specifics surrounding this topic.
What is gastroparesis?
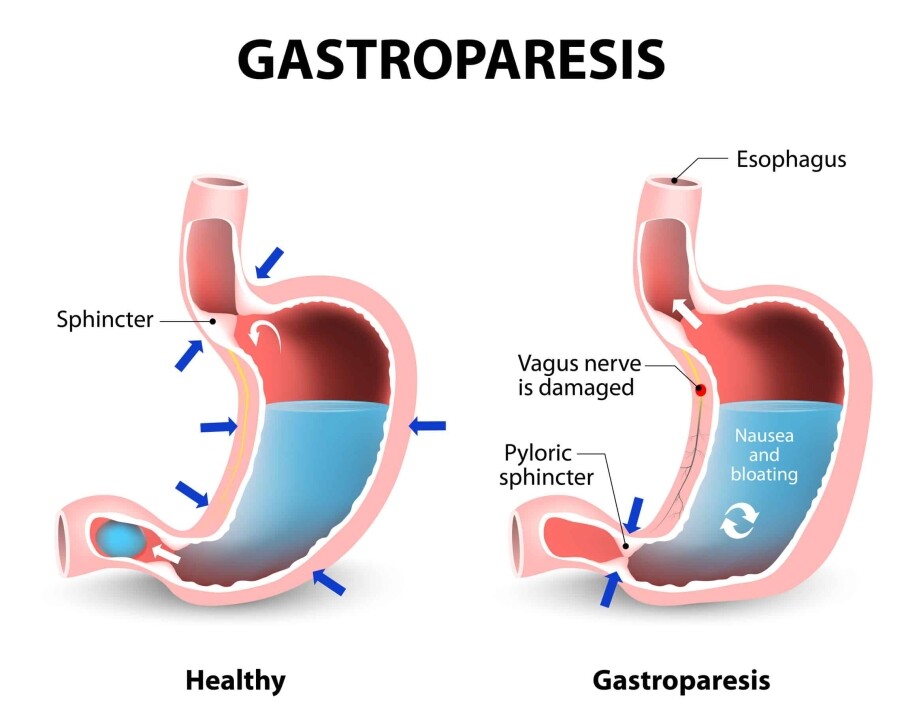
The digestive system can be complex and proper function is crucial for a person maintaining their health. Typically, muscle contractions in the stomach and intestines help move food through the digestive system.
However, gastroparesis is a condition that slows down or stops the stomach’s muscular contractions. This means that food will stay in the stomach longer than usual instead of moving into your small intestines.
The exact cause of gastroparesis is not always known. Some medications, such as those opioids, antidepressants, high blood pressure meds, and allergy drugs, can cause symptoms of this condition.
However, diabetes appears to one of the most common causes.
How does diabetes cause gastroparesis?
Gastroparesis often occurs in those with type 1 and type 2 diabetes, which is why it is frequently referred to as diabetic gastroparesis.
Diabetes can cause a variety of complications. One of these complications is nerve damage.
Chronically high blood sugar levels can damage nerves and can cause chemical changes in the nerves. In the same way, high blood sugar can damage blood vessels responsible for supplying the nerves with nutrients.
When it comes to the digestive system, diabetes can damage the vagus nerve. The vagus nerve plays a crucial role in controlling the movement of food through the digestive tract.
If the vagus nerve becomes damaged, the muscles in the stomach and intestines will not function properly. Thus, food remains in the stomach longer than normal and moves slower through the digestive tract.
When food is slowed or stopped from moving through the stomach or intestines, various symptoms can occur.
Diagnosing diabetic gastroparesis
There are a few different tests that doctors may use for properly diagnosing gastroparesis.
There are two types of gastric emptying tests, which include:
- Scintigraphy – This includes consuming a small meal that contains a minimal amount of radioactive material. A scanner used for detecting radioactive material is then used to monitor how quickly food moves through the stomach.
- Breath tests – This test involves consuming food with a specific substance that becomes detectable in your breath. The substance in your breath is then detected and measured at different intervals of time. This helps determine how quickly food is moving through your stomach.
An upper gastrointestinal (GI) endoscopy is another test that uses a small camera at the end of a thin, flexible tube to visually examine the upper portion of the digestive system.
Lastly, an ultrasound could be used to rule out other problems that could potentially be causing your symptoms.
Diabetic gastroparesis symptoms
Symptoms of diabetic gastroparesis may include:
- Nausea
- Heartburn
- Vomiting undigested food
- Feeling full earlier than normal
- Feeling full long after eating
- Weight loss
- Bloating
- Fluctuating blood sugar levels
- Decreased appetite
- Acid reflux or GERD
- Spasms in the stomach
- Chronic abdominal pain
Diabetic gastroparesis complications
Diabetic gastroparesis can lead to a variety of complications. One of the more obvious complications is that it can make your diabetes more difficult to manage.
Food staying in the stomach longer than normal makes it difficult to determine when to inject your insulin. This can lead to an increased risk of having too many high or low blood sugar levels, which has additional complications.
For example, high blood sugar levels can lead to:
- Kidney problems
- Heart disease
- Eye damage (retinopathy)
- Foot problems
- Neuropathy
- Ketoacidosis
Untreated low blood sugar can lead to:
- Shakiness
- Nervousness
- Unconsciousness
- Seizures
Other complications of diabetic gastroparesis may include:
- Bacterial growth due to food staying in the stomach too long. Food that remains in the stomach for too long can ferment, leading to the growth of bacteria.
- Bezoars due to food hardening in the stomach. This can lead to a blockage of the stomach preventing food from passing into the small intestines. Bezoars can cause nausea and vomiting.
- Malnutrition
- Dehydration
- Imbalance of electrolytes
- Esophagus tears due to excessive vomiting
- Inflammation of the esophagus, which can make swallowing difficult
- Low quality of life. Symptoms can make it difficult to work and perform daily functions.
Diabetic gastroparesis treatment
Treating gastroparesis is often done by treating the underlying condition. For example, if diabetes has caused this digestive problem, then treating your diabetes condition is one step to take for treatment.
More specifically, changing your diet may be able to help you relieve symptoms of diabetic gastroparesis.
Diabetic gastroparesis diet
If you have gastroparesis, you should focus on getting the nutrition you need while eating smaller but more frequent meals. The types of foods you are consuming should also be easy to digest.
Here is a list of foods to eat to help with diabetic gastroparesis:
- Eggs
- Lean beef or pork
- Chicken without the skin
- Lean fish
- Peanut butter
- Bananas
- Hot cereals
- Crackers
- Vegetable juice
- Cooked vegetables without the skin
- Fat-free products
Foods to avoid:
- 2% milk and other dairy products
- Cheeses
- Canned beef, hot dogs, bacon, sausage, etc.
- Beans
- Liquid oils and fats
- Raw vegetables
- Cakes, pies, ice cream
- Nuts
- High-fiber foods
- Alcohol
Practical Tips
Along with this list of foods to eat and avoid, patients should ensure they drink plenty of water. This will help them avoid dehydration.
When drinking fluids, do not gulp large amounts at one time. Instead, sip on water steadily throughout the day.
It is recommended that you sit straight up or stand while eating and for at least one hour after.
Exercise has been proven to improve digestion and stomach emptying. Try going on a walk after your meals.
Reducing your fiber intake may help. Fiber often slows the digestion process further and can cause bezoars when eaten while you have gastroparesis.
Chew your foods well. Blending your foods may prove to be most beneficial.
Related: 5 Fruits Diabetics Should Avoid
Medications
There are medications available to help you deal with the symptoms of diabetic gastroparesis. These medications may include:
- Metoclopramide – This medication stimulates the muscles of the stomach wall, causing a contraction. This can improve gastric emptying, as well as prevent nausea and vomiting. Reglan is the brand name version.
- Domperidone – This medicine works similarly, causing contractions in the stomach muscles. Nausea and vomiting can be relieved with domperidone, but the medication is only available under a special program due to its potential side effects.
- Erythromycin – This is an antibiotic medication but is also a gut stimulator, which improves gastric emptying.
- Antiemetics – This medicine is often prescribed for preventing motion sickness. It can provide relief from nausea and vomiting.
- Antidepressants – Antidepressants may be able to help you deal with nausea and vomiting. However, they may not actually help your condition improve.
- Pain medicines – Pain in your abdomen from diabetic gastroparesis may be reduced by certain non-narcotic pain medicines.
Surgery
Some patients may need surgical intervention if they are unable to tolerate food or liquids.
In severe cases, doctors may recommend intervention with the use of a feeding tube. A feeding tube is placed directly into the small intestines.
Another surgical intervention includes inserting a gastric venting tube. This is a tube placed in the stomach and relieves nausea and vomiting by draining the stomach of fluids.
Final thoughts
We hope this has provided you more insight into diabetic gastroparesis. Please note that this article is not meant for medical guidance. Always consult your doctor regarding your specific medical condition and treatment options.
If you are struggling to afford your prescription medications, then Prescription Hope may be able to help. Our advocates work with doctors, pharmacies, and even pharmaceutical manufacturers to assist patients in getting their medications at an affordable cost. Enroll with us and start paying just $70.00 a month through Prescription Hope’s medication access service for each of your prescription drugs.